The CMS 5 Star Ratings system is a quality measurement tool designed by the Centers for Medicare & Medicaid Services (CMS) to assess the performance of Medicare Advantage plans.
A plan’s star rating is a critical measure that affects not only compliance but also reimbursement bonuses and member enrollment. Continuous star rating monitoring and improvement by a qualified firm such as HDC, will help avoid costly penalties if a plan’s star rating is negatively impacted.
Recent changes in Star Methodology can, and have, caused health plans to lose billions of dollars. Protect yourself from these losses by working with HDC to both monitor and improve your star ratings.
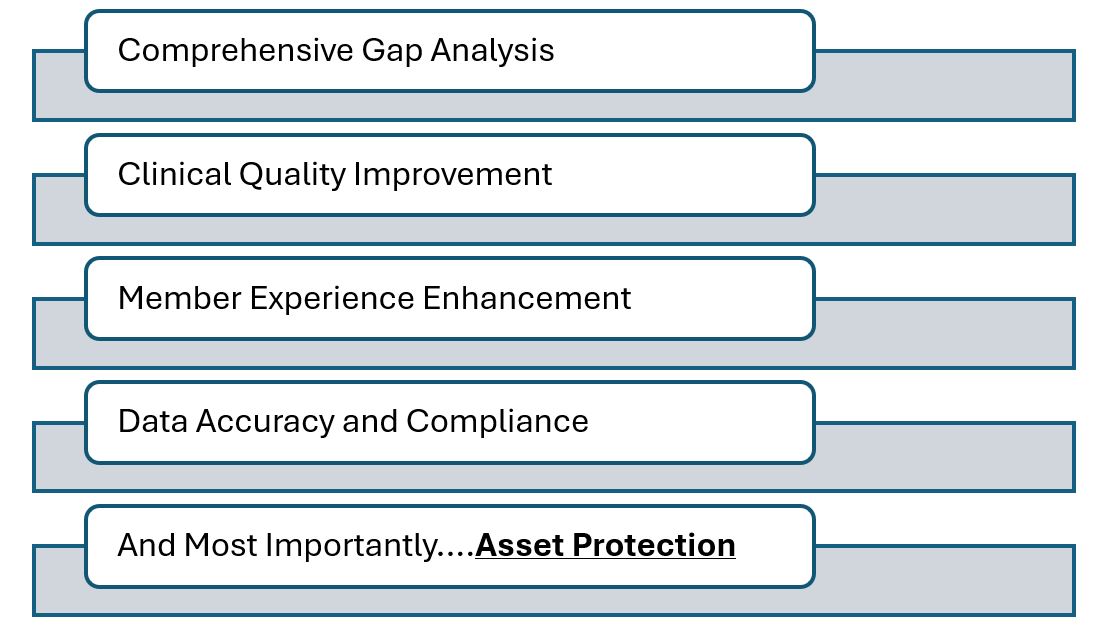
HDC has years of experience in healthcare quality, compliance, and analytics. Our team delivers customized strategies to help your organization meet and exceed current star rating goals. Our services include, but are not limited to: